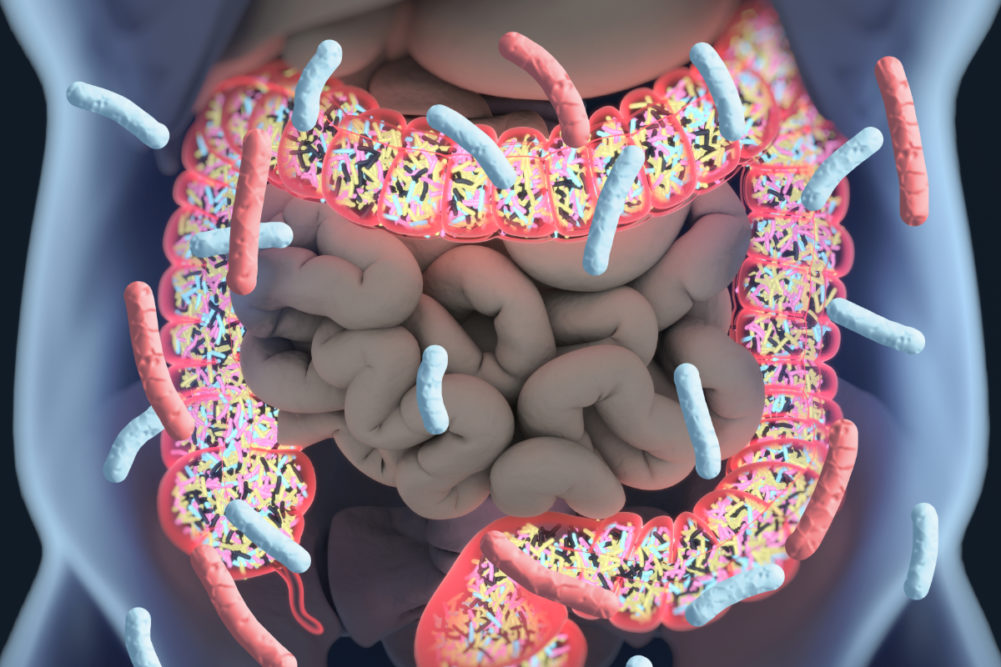
Two studies published this year revealed new findings on the human gut microbiome. One linked the composition of patients’ gut microbiota to how severe their case of COVID-19 was. The other study found a link between processed food and the microbiome.
A study that appeared online Jan. 11 in Gut Microbiota suggested the gut microbiome is involved in the magnitude of COVID-19 severity. Researchers from the Chinese University of Hong Kong in February and May of last year collected blood and stool samples from 100 patients with SARS-CoV-2 infection (the virus that causes COVID-19).
Gut microbiome composition was altered significantly in patients with COVID-19 compared with 78 adults who were in a control cohort and did not have COVID-19. Faecalibacterium prausnitzii, Eubacterium rectale and bifidobacteria, which all have immunomodulatory potential, were underrepresented in patients with COVID-19.
The other study was published online Jan. 11 in Nature Medicine and uncovered links between a person’s diet, the microbiome (microbes in their gut) and their health. Researchers investigated 1,203 gut microbiomes from 1,098 individuals enrolled in the Personalized Responses to Dietary Composition Trial (PREDICT 1) study and identified microbes that positively or negatively correlate with an individual’s risk of serious conditions such as diabetes and heart disease.
As an example of a positive correlation, a microbiome rich in Prevotella copri and Blastocystis species was associated with maintaining a favorable blood sugar level after a meal. Subjects who ate a diet rich in healthy, plant-based foods were more likely to have high levels of “good” gut microbes.
As an example of a negative correlation, the researchers found microbiome-based biomarkers of obesity, cardiovascular disease and impaired glucose tolerance, all of which are key risk factors for COVID-19. Diets containing more highly processed plant-based foods were more likely to be associated with the “bad” gut microbes.
“We were surprised to see such large, clear groups of what we informally call ‘good’ and ‘bad’ microbes emerging from our analysis,” said Nicola Segata, PhD, professor and principal investigator of the Computational Metagenomics Lab at the University of Trento in Italy and leader of the microbiome analysis in the study. “It is also exciting to see that microbiologists know so little about many of these microbes that they are not even named yet. This is now a big area of focus for us, as we believe they may open new insights in the future into how we could use the gut microbiome as a modifiable target to improve human metabolism and health.”
The study involved researchers from King’s College London, the Harvard T.H. Chan School of Public Health in Boston, Massachusetts General Hospital in Boston and the University of Trento in Italy.